When it comes to finding a cure for Parkinson’s disease, developing a way to shield vulnerable brain cells from damage is at the top of the list.
That’s because the progressive loss of these critical cells—and the resulting lack of a neurotransmitter they produce called dopamine—triggers the disease’s hallmark symptoms, which eventually robs people with Parkinson’s of their ability to move.
“A therapy that can slow or stop cell damage or, even better, prevent it from occurring in the first place, would completely revolutionize Parkinson’s care,” said Dr. Patrik Brundin, associate director of research at Van Andel Research Institute (VARI). “It would shift treatment from reactive symptom management to proactive prevention. That would be a game-changer.”
Therapies such as those Brundin describes are sorely needed. An estimated seven to 10 million people worldwide have Parkinson’s, a number that is expected to increase as the global population ages. At the same time, current treatment options only help mitigate symptoms, rather than slow or stop the course of the disease.
So far, most attempts aimed at protecting the brain cells impacted by Parkinson’s have focused on singular components underlying the disease, ultimately failing once they reach human clinical trials.
Now, a collaborative team spearheaded by Brundin, Dr. Merritt DeLano-Taylor at Grand Valley State University and Dr. Jeffrey Kordower at Rush University and VARI, is taking a new approach—activating multiple molecular pathways that have been shown to defend cells against the toxic proteins that cause the disease.
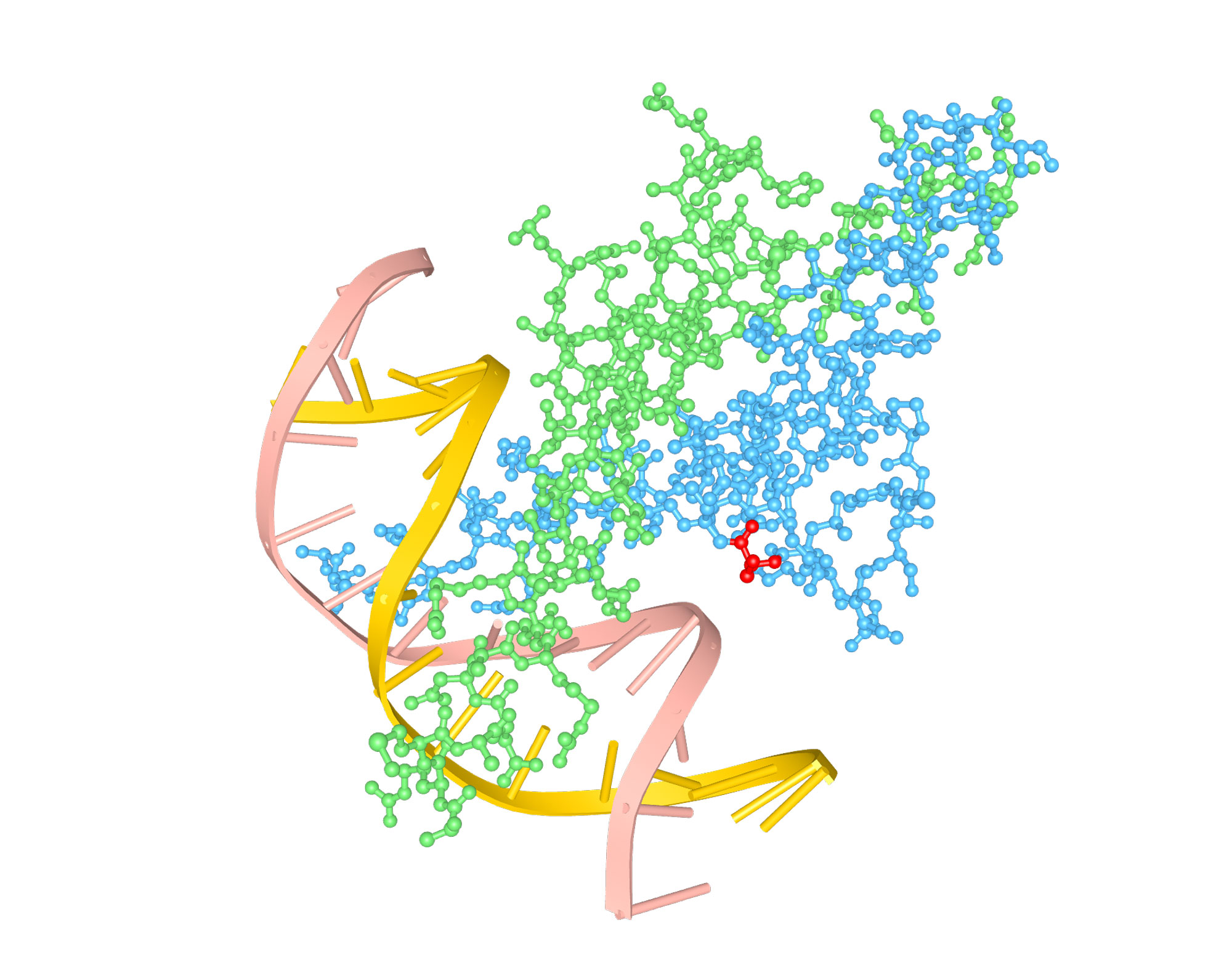
Their tool? A modified version of a different protein with a name straight out of the Star Wars universe: PM-Nato3.
“PM-Nato3 can drive the expression of many factors that have been shown to protect dopamine neurons from disease,” said DeLano-Taylor. “It may be a useful tool because instead of relying on a single factor to protect the neurons, we may be able to activate an armada of these factors, increasing the likelihood of survival and therapeutic benefit.”
The patent-pending PM-Nato3 technology was developed by Grand Valley alumni Nicholas Huisingh, Jordan Straight, Daniel Doyle and Douglas Peterson while they were undergraduate students.
The team is testing its hypothesis in several laboratory models of the disease thanks to a two-year, $500,000 award from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health. Brundin, DeLano-Taylor and Kordower hope to sort out exactly how PM-Nato3 works and how their findings can be used to develop potential new therapies.
“This work represents the exciting first steps of an approach that has never before been attempted—the coordinated activation of multiple protective pathways in Parkinson’s,” Kordower said. “We are cautiously optimistic and hope that our findings change Parkinson’s treatment for the better.”
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number R21NS105436. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.