In honor of Parkinson’s Awareness Month and the 200th anniversary of Dr. James Parkinson’s An Essay on the Shaking Palsy, we asked scientists in our Center for Neurodegenerative Science about the most exciting things happening right now in Parkinson’s research. Here’s what they said.
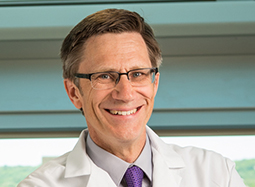
 Dr. Patrik Brundin
Dr. Patrik Brundin
Associate Director of Research
Director, Center for Neurodegenerative Science
Although we’ve come a long way since An Essay on the Shaking Palsy in 1817, there is still much to be done. The last few years of Parkinson’s research in particular have been especially heartening. From the promise of drug repurposing to discovering potential new biomarkers, we are well on the way to finding better ways to not only diagnose Parkinson’s but to slow or stop it and to repair the damage it causes in the brain. This work is important, urgent and—for the seven to 10 million people globally with the disease, their families, their friends and the movement disorders community—deeply personal. We will accept nothing less than life changing-treatments and, ultimately, a cure.
 Dr. Lena Brundin
Dr. Lena Brundin
Associate Professor
Although Parkinson’s is largely recognized as a disease that affects movement, there are many other non-motor symptoms, such as depression, that can also be debilitating. Our work has revealed that elevated levels of chemicals associated with inflammation may serve as biomarkers for depression, which may one day help us better diagnose, monitor and treat it. We also are investigating whether inflammation in the brain damages the neurons associated with Parkinson’s, contributing to the disease’s motor symptoms as well as depression. By developing a clearer picture of the relationship between these conditions and inflammation, we hope this work will be a game-changer that will help scientists to better study the disease and for physicians to better treat patients on a case by case basis.
 Dr. Gerhard (Gerry) Coetzee
Dr. Gerhard (Gerry) Coetzee
Professor
Our lab is interested in genetic risk factors influencing Parkinson’s, particularly small changes to the genome that may not cause problems on their own but when taken together or with environmental factors, may increase a person’s likelihood of developing the disease. We recently discovered some of these small changes, which are called SNPs, in a few surprising areas, namely immune, skin, liver and fat cells, in addition to brain cells. Many of these SNPs were also linked to genes that are associated with inflammation, the body’s response to an injury, infection or other insult. In short, this means that other areas outside of the brain may play important roles in Parkinson’s risk while also reinforcing the role of inflammation as a driver for the disease. We’re excited to continue investigating these findings, which hold promise for revealing new targets for treatment.
 Dr. Jeffrey Kordower
Dr. Jeffrey Kordower
Director’s Scholar, Van Andel Research Institute
Alla V. and Solomon Jesmer Professor of Neurosciences, Rush University Medical Center
One of the biggest challenges in Parkinson’s treatment is the lack of therapies that actually interferes with the disease’s progress or that repairs the damage to the brain. However, I think that this could soon change. We know more about Parkinson’s now than ever before and, together with colleagues around the world, are working to translate this insight into innovative new ways to restore lost function. There is a tremendous sense in the scientific and patient communities that we are drawing close to a paradigm-shift in the way we treat Parkinson’s.
 Dr. Viviane Labrie
Dr. Viviane Labrie
Assistant Professor
For a long time, much of our genetic code was thought to be junk. The realization that these previously disregarded DNA regions act like a volume dial for gene expression was revolutionary. However, there is a gatekeeper to the activity of such DNA regions—the epigenetic code—which is an important regulator of genomic activities, and consequently affects how cells function and age. We’re looking at how the epigenetic code, particularly at these previously ignored DNA regions, impacts the onset of Parkinson’s and Alzheimer’s diseases. We are also studying how aging, which is the biggest risk factor for both diseases, impacts disease development. Looking at epigenetics in neurodegeneration is a relatively new field but it holds untold promise for better understanding the disease and ultimately finding new ways to slow or stop it.
 Dr. Jiyan Ma
Dr. Jiyan Ma
Professor
In order to one day stop Parkinson’s disease progression, we need to understand in intricate detail how it spreads from cell to cell in the brain. The field now better appreciates that abnormal alpha-synuclein, the protein found in all cases of Parkinson’s, is capable of traveling throughout the nervous system and to the brain from other places in the body. These realizations have revolutionized the field and given us new avenues to explore in our search for life-changing therapies.
 Dr. Darren Moore
Dr. Darren Moore
Associate Professor
The emergence of the endolysosomal pathway—otherwise known as cells’ recycling and housekeeping system—as a common mechanism underlying the development of Parkinson’s is one of the most exciting developments in neurodegenerative disease research. Many genes and risk factors associated with Parkinson’s appear to be related to this fundamental cellular pathway, which is responsible for clearing cellular debris and defective proteins out of cells, keeping them healthy and functioning normally. Understanding how problems with this process are related to Parkinson’s holds tremendous promise for the development of new ways to treat the disease. In fact, our 2016 Grand Challenges in Parkinson’s Disease symposium was entirely devoted to this new exciting topic. Our lab is actively working to make breakthroughs, which could really change how we view and treat Parkinson’s.

Dr. Jeremy Van Raamsdonk
Assistant Professor
While aging has long been known to be the greatest risk factor for the development of Parkinson’s, the role it plays in the disease remains poorly defined. Our recent work suggests that targeting molecular pathways that are associated with aging can increase the survival of brain cells in models of Parkinson’s. As there are currently no therapies for the disease that can protect brain cells from death, this work could potentially lead to a novel treatment.