Combining epigenetic cancer medications may have benefit for colorectal cancers and other tumor types
March 27, 2024
GRAND RAPIDS, Mich. (March 27, 2024) — A pair of medications that make malignant cells act as if they have a virus could hold new promise for treating colorectal cancers and other solid tumors, reports a study published today in Science Advances.
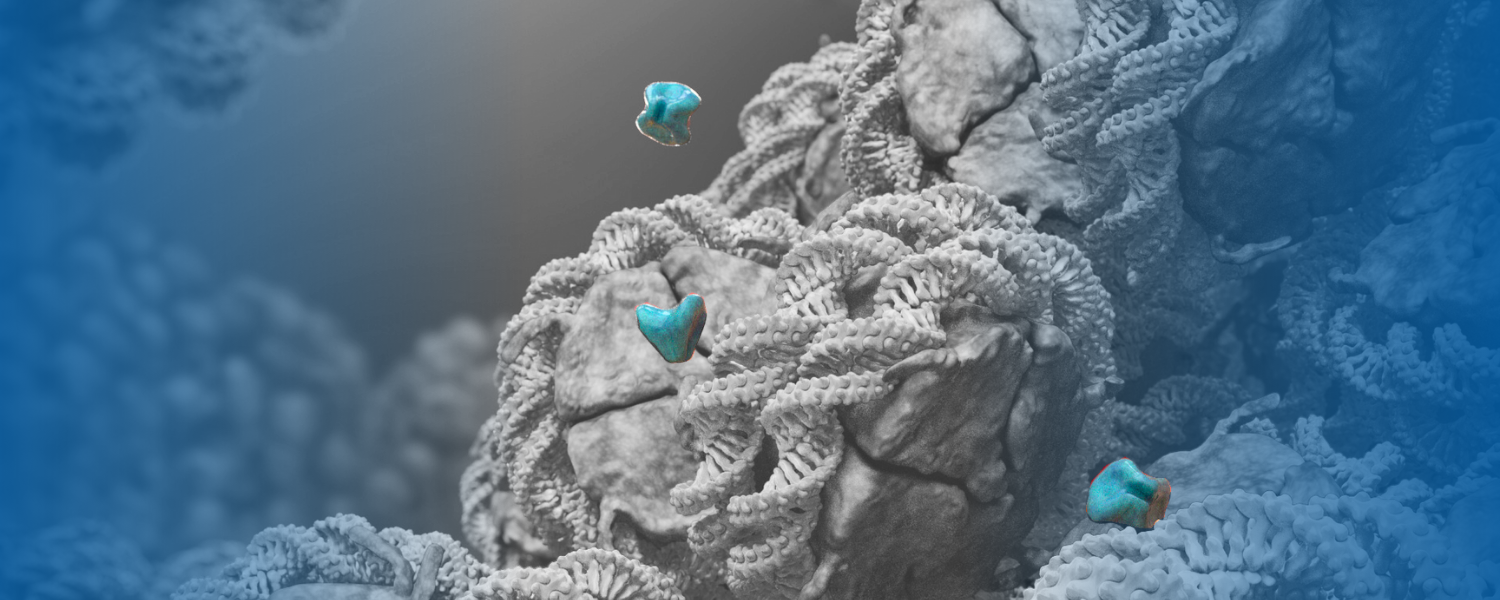
The preclinical research, led by Van Andel Institute scientists, determined how low doses of a DNMT inhibitor sensitize cancer cells to an EZH2 inhibitor, resulting in a one-two punch that combats cancer cells better than either drug alone.
The findings are the foundation for an upcoming Phase I clinical trial to evaluate this combination in people with colorectal cancer or other solid tumors.
“DNMT inhibitors are approved to treat blood cancer while EZH2 inhibitors are approved to treat blood cancer and a rare type of sarcoma. To date, they’ve had limited individual success in solid tumors like colorectal cancer,” said Van Andel Institute Professor Scott Rothbart, Ph.D., the study’s corresponding author. “Our findings highlight the promise of combination cancer therapies by revealing how these two medications interact, with the DNMT inhibitor priming cancer cells in a way that makes the EZH2 inhibitor more effective.”

DNMT and EZH2 inhibitors work by controlling the epigenetic processes that regulate gene expression. In cancer, epigenetic errors enable malignant cells to survive and proliferate — and offer critical targets for treatment.
Previous studies show that DNMT inhibitors cause cancer cells to behave as if infected by a virus, which makes the cells more susceptible to attack by one’s own immune system. In their new study, Rothbart and colleagues demonstrated that combining DNMT and EZH2 inhibitors activate this viral mimicry process more effectively than either drug on its own. The upcoming trial will be the first time these two medication types will be combined to enhance the activities of these inhibitors in solid tumors.
Colorectal cancers are the second leading cause of cancer death globally, according to the World Health Organization. More than 1.9 million cases were diagnosed in 2020, with incidence expected to rise to 3.2 million cases by 2040. Although screening and early detection have driven down colorectal cancer rates among older people in the U.S., rates are rising in younger people.
“Although it is not clear why colorectal cancer cases are rising among young people, it is clear that we need more effective treatment strategies,” Rothbart said. “Combining medications may be a powerful way to simultaneously target multiple drivers of cancer. In addition to revealing how DNMT and EZH2 inhibitors work together, our findings suggest that epigenetic drugs also may sensitize tumors to immunotherapy, which offers another important opportunity to enhance cancer treatment.”
Related: Learn more about the Rothbart Lab ➔
The upcoming trial will be supported by the Van Andel Institute–Stand Up To Cancer© (SU2C) Epigenetics Dream Team, a multi-institutional collaboration that evaluates promising potential combination therapies for cancer, and a National Cancer Institute Specialized Programs of Research Excellence (SPORE) award, a prestigious five-year grant that supports a team of scientists seeking to improve epigenetic cancer therapies.
Today’s findings were made possible in part by a SPORE-supported subproject on DNMT and EZH2 inhibitors led by Rothbart and Stephen Baylin, M.D., of Johns Hopkins University and Van Andel Institute. Baylin also serves as co-leader of the VAI–SU2C Epigenetics Dream Team and is an author on today’s study.
The study’s first authors are Alison A. Chomiak, Ph.D., and Rochelle L. Tiedemann, Ph.D., of VAI. Other authors include Yanqing Liu, M.D., Ashley K. Wiseman, M.S., and Kate E. Thurlow, M.Sc., of VAI; Xiangqian Kong, Ph.D., Ying Cui, Ph.D., and Michael E. Topper, Ph.D., of Johns Hopkins University; and Evan M. Cornett, Ph.D., of Indiana University.
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award nos. P50CA254897 (Issa, Baylin and Jones; sub-project 7830, Rothbart) and F32CA225043 (Chomiak); and the National Institute of General Medical Sciences of the National Institutes of Health under award no. R35GM124736 (Rothbart). Scott Rothbart, Ph.D., was supported by a Research Scholar Grant (RSG-21-031-01-DMC) from the American Cancer Society. Rochelle L. Tiedemann, Ph.D., was supported by the American Cancer Society–Michigan Cancer Research Fund Postdoctoral Fellowship (PF-16-245-01-DMC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders.
